Health economics
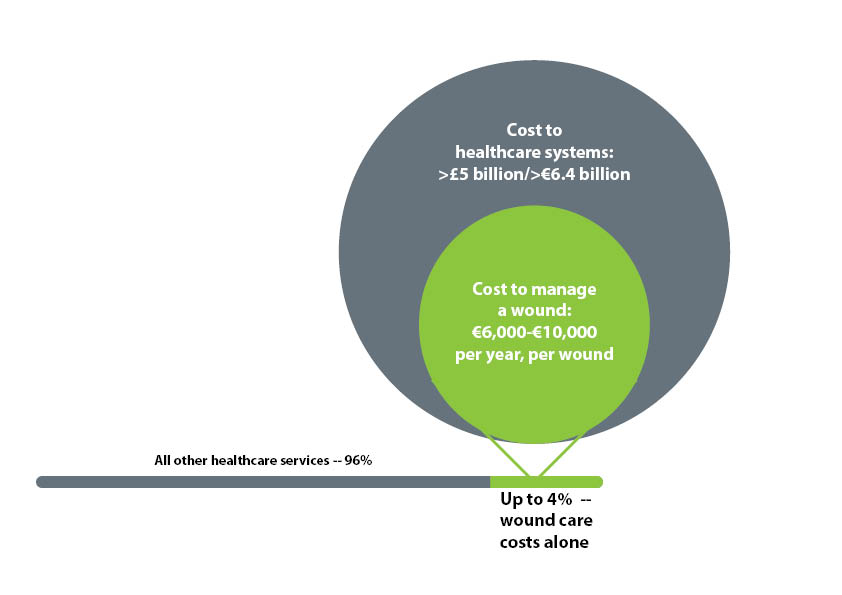
The cost of treating chronic wounds is significant. It’s estimated that, across Europe, 2-4% of healthcare expenditure is spent on wounds, and this figure is on the rise[1–3]. The average cost of treating a wound ranges from about €6,000–€10,000 per year[3]. In the UK, up to more than £5 billion (€6.4 billion) is spent on treating wounds annually, based on current local healthcare budget projections[4].
Spiralling costs
Going forward, costs have the potential to spiral, as the population is increasingly made up of older people, with greater prevalence of co-morbid conditions[5]. In fact, patients with multiple long-term conditions, such as diabetes, vascular disease and obesity, are “becoming the norm rather than the exception and the number of people with co-morbidities is set to increase”[6]. Furthermore, as the population of Europe ages and the incidence of co-morbid conditions that give rise to wounds increases, costs are likely to rise accordingly[7].
Further complications
Wounds that are stalled are more likely to develop complications, such as infection, which in turn require more-costly interventions and more-frequent dressing changes, both of which place greater demands on our limited resources[8]. Wound complications contribute to longer and more intensive treatment, extended hospital stays, readmission, and specialist medical or even surgical intervention[8]. These costs can continue to pile up if stays are prolonged because there are not adequate systems to facilitate early discharge, or there is a “perceived or actual lack of capacity and capability to manage more complex wounds in the community setting”[8]. In fact, it is estimated that between 25–50% of acute hospital beds are occupied by patients with a wound[3].
When patients are discharged into the community, hard-to-heal wounds pose further costs in terms of the duration of treatment required. The longer the time to healing, the greater the need for dressing changes on a regular basis, which requires significant health provision time on the parts of community and practice nurses[8]. In one study in Sweden in a community of 288,000 with a typical wound prevalence of 2.4 per 1000 population, the equivalent of 57 full-time nurses were required for dressing changes alone[9].
Wound management
Therefore, it is critically important to choose the right dressing at the right time. That is, using the most clinically effective dressing for the wound, particularly for hard-to-heal and stalled wounds. The wound management regimen should help control symptoms, promote wound closure and improve quality of life, while generating long-term savings by minimising nursing visits or use of specialist time, preventing infection (or, later, amputation)[10].
Woulgan Bioactive Beta-Glucan Gel brings savings
Economic modelling shows that the wound-healing efficacy of appropriately using Woulgan Bioactive Beta-Glucan Gel advanced wound dressing imparts significant savings when compared to using standard dressings (figure 1).
Figure 2. Treatment cost in trial population*[11]
| WOULGAN | Std. care | Difference | |
|---|---|---|---|
| Average treatment cost per healed ulcer | |||
| 12 weeks 52 weeks** |
£2,628 £3,378 |
£3,706 £4,762 |
-£1,078- £1,384 |
| Average treatment cost to reach standard of care healing rate (37%) | |||
| £830 | £1,359 | -£529 | |
**Calculated from extrapolated data of PP population
Because Woulgan is intended for use on hard-to-heal and stalled wounds, the long-term savings across the healthcare system could be even greater. A full analysis has been published in JWC (Journal of Wound Care) 2017: “The cost-effectiveness of a novel soluble beta-glucan gel”.
Patient quality of life
Hard-to-heal and stalled wounds can have a devastating impact on patient well-being that reaches far beyond the healthcare system and can compound healthcare costs. Although patients living with a wound are concerned with long-term healing, they may be more focused in the short term on reducing pain or odour, or being able to participate in their usual daily activities[12].
Patients who cannot maintain or increase activity levels may experience a deterioration in the status of their wounds (e.g. where mobility is part of managing co-morbid conditions). Anxiety and depression are associated with the long treatment durations of stalled wounds and patients may become non-concordant with their care[12]. In such cases, the need for more intensive wound management therapies or the use of other services (e.g. mental health) may further strain the healthcare system.
Summary
Woulgan is a gel that is comfortable for patients. It helps to stimulate patients’ immune response, which can lead to faster healing in wounds that have become — or are at risk of becoming — stalled. These factors can help increase patient satisfaction and, in turn, encourage them to keep up with their care regimens — which not only addresses quality-of-life issues, but also has the potential to help save resources for the healthcare system.
References
- Purwins S, Herberger K, Debus S, et al. Cost-of-illness of chronic leg ulcers in Germany. Int Wound J. 2010;7(2):97–102.
- Hjort A, Gottrup F. Cost of wound treatment to increase significantly in Denmark over the next decade. J Wound Care. 2010;19(5):173–4, 176, 178, 180, 182, 184.
- Posnett J, Gottrup F, Lundgren H, Saal G. The resource impact of wounds on health-care providers in Europe. J Wound Care. 2009;18(4):154–161.1.
- Using Nanova Therapy System in Practice: a round table discussion. London: Wounds UK. 2015;11(4):Supplement
- Department of Health (DOH). Comorbidities: A framework of principles for system-wide action. London: DOH, 2014. Accessed November 2015 at: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/307143/Comorbidities_framework.pdf
- Department of Health (DOH). Long term conditions compendium of information: third edition. London: DOH, 2012. Accessed November 2015 at: https://www.gov.uk/government/publications/long-term-conditions-compendium-of-information-third-edition
- Moore ZE, Cowman S. Repositioning for treating pressure ulcers. Cochrane Database Syst Rev. 2009 Apr 15;(2):CD006898. doi: 10.1002/14651858.CD006898.pub2.
- Dowsett C. Breaking the cycle of hard to heal wounds: balancing cost and care. Wounds Int 2015;6(2):17–21
- Lindholm C, Bergsten A, Berglund E. Chronic wounds and nursing care. J Wound Care 1999;8(1):5–10
- Vowden P. Hard-to-heal wounds Made Easy. Wounds Int 2011;2(4)
- Zykova SN, Balandina KA, Vorkohobina N, et al. Macrophage stimulating agent soluble yeast β-1,3/1,6-glucan as a topical treatment of diabetic foot and leg ulcers: A randomized, double blind, placebo-controlled phase II study. J Diabetes Invest 2014;5(4):392–9
- International consensus. Optimising wellbeing in people living with a wound: An expert working group review. London: Wounds International, 2012.