Wound healing comes with a variety of potential complications. Aside from infection, these can include tissue overgranulation, necrosis and potentially chronic discomfort.(1,2).
Although not all these complications are always preventable, it is important to treat them early if they arise. Therefore such complications should be considered for wounds of all origins, be they trauma or disease associated, or resulting from surgery.
Wounds with minimal tissue loss, such as those from surgery, can be categorized as ‘primary’, while those with substantial tissue loss, such as ulcers, are categorized as ‘secondary’ and may undergo a less predictable healing process.(2)
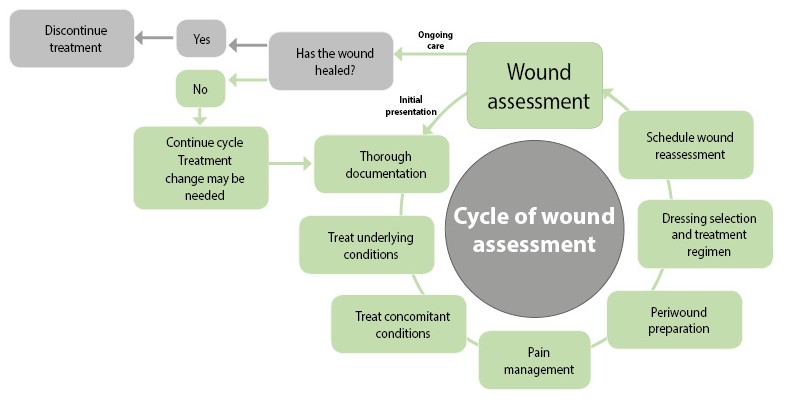
Thorough, holistic assessment and reassessment are key for preempting complications, providing initial appropriate wound treatment, and adapting treatment as the wound evolves.(2)
Although initial wound assessment is recognized as important, current practice in re-assessment and documentation may be less effective.(2)
What is good wound assessment?
The aim of the initial assessment of a wound is to obtain a correct diagnosis and find appropriate treatment.(2) The accuracy of this assessment is vital for wound management to be successful.(2) For some wounds, particularly chronic ones, a differential diagnosis may be needed.(2)
Therefore knowledge of pathophysiology, physiology and anatomy are needed in addition to an understanding of the healing process(2), and a multidisciplinary approach may be required.(3)
Wound assessment should be holistic and account for all possible factors that might influence wound healing.
This includes a review of patient lifestyle, psychosocial needs/support, and general health — for example, the presence of concurrent disease such as diabetes, infections, nutritional status and current medications.(2)
Tools have been developed to facilitate systematic assessment. These include NHS wound assessment charts and the ‘TIME’ approach (Tissue-Infection-Moisture-Edge).(1,4)
These assessments involve review of the appearance of the wound but also pain, which can be an indicator of infection and inflammation, and the impact of the wound on quality of life.(1, 2) The assessment should provide the basis for appropriate treatment decisions.
These decisions should encompass cleansing of the wound, the choice of dressing and its properties, pain management, and any additional treatment required such as administration of antibiotics.(1)
Holistic assessment should also guide complementary and multidisciplinary management approaches, such as skin care, referral to a vascular surgeon if needed, and advice for appropriate physical activity.
Initial assessment is only the beginning
Adequate assessment is not complete without thorough re-assessment and documentation.(2) This is particularly important for determining if progression or deterioration of the wound is occurring.(2)
A wound might be expected to follow characterised stages of healing — haemostasis, inflammation, proliferation and epithelialisation.(2) However, regular reassessment of the wound and the treatment approach over time will highlight if this healing process is not happening.
In particular, chronic wounds such as diabetic foot ulcers may not follow this classical sequence of healing events.(3)
Reassessment of a wound should also take place if the patient’s condition changes, for example if health or disease deteriorates, or if medication is altered.(3) The timing of reassessment is dependent on the nature of the wound.
In some cases, biopsy and histological diagnosis may be needed as part of the reassessment.(3)
Adequate documentation is needed in order to review the previous status of a wound and the history of management and treatment.(1) This documentation might be necessary to track an absence of signs of healing and to form a basis for future care.(3)
In cases of inadequate wound healing, correct documentation can reveal areas of practice that need to be improved.(2) For compliance with best practice, correct documentation is therefore required.(1,2)
A wound can be defined as ‘a break in the continuity of the skin’ and therefore these principles of wound assessment and care can apply to a wide range of acute and chronic conditions.(3,4)
A standardised and systematic approach to wound assessment at regular intervals is vital for recognising when changes in wound care need to be made.
References
- Guidelines for the assessment and management of wounds. Northamptonshire Healthcare NHS Foundation Trust. 2015.
- Stephen-Haynes J. Wound assessment in the primary care setting. Community Health & Care Support.
- National best practice and evidence based guidelines for wound management. Health Service Executive. 2009.
- Schultz GS, Sibbald RG, Falanga V, Ayello EA, Dowsett C, Harding K, et al. Wound bed preparation: a systematic approach to wound management. Wound Repair Regen 2003;11 Suppl 1:S1-28.
This information helped me so much to complete my school assignment, and I found everything that I needed. Thanks.