When wound healing stalls, patients experience lower quality of life, clinician time increases exponentially, and healthcare systems spend precious resources to provide care that usually could have been prevented. This overview explores wound-healing, defines types of challenging wounds, and examines the effects of stalled wound healing on health systems and patients.
Stages of wound healing
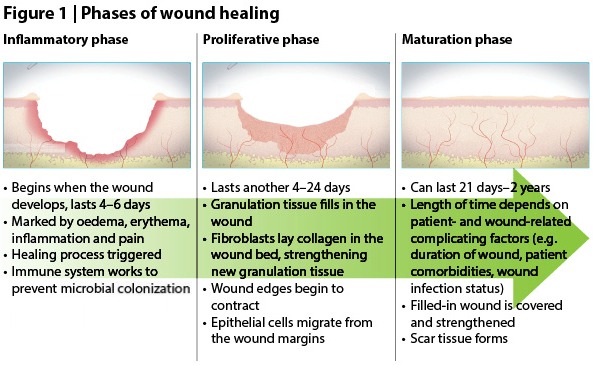
Broadly, wounds progress through three phases of healing (see Figure 1)
Differentiating challenging wounds
Thorough, holistic wound assessment will help you differentiate complicated wounds — those that might have an issue healing according to the normal trajectory. Here are three types, and how we’ll be using them over the course of the blog.
| Timeline of diagnosis | Type of challenging wound | Short description |
|---|---|---|
| Determined at initial presentation | Hard-to-heal | Patient or wound factors make it likely that the wound will fail to heal with standard therapy in an orderly and timely manner. Assessment at presentation of a new wound should focus on identifying these wounds, to ensure they are managed appropriately from the outset. Wounds that have stalled or become chronic — that is, have already failed to heal in a straightforward way — are also considered hard-to-heal.[2] |
| Can be determined at any point along the healing trajectory | Stalled | The wound initially began to heal, but patient- or wound-related factors have prevented the wound from continuing to heal in an orderly and timely manner. The wound is stuck — ‘stalled’ — in the inflammatory phase, requiring advanced management to restart healing. A good rule of thumb to follow: If the wound has not healed by 40% after 4 weeks, it should be considered stalled.[3,4] |
| Determined 8–12 weeks from initial presentation | Chronic | The wound has been present for 8–12 weeks. It may have become stalled at any point, from initial presentation to near-closure. These wounds require advanced management to restart healing and/or achieve closure.[5] |
A closer look at stalled wounds
Wounds may become stalled at the inflammation phase, exhibiting low-grade inflammation for a long period of time (sometimes indefinitely) for a number of patient- or wound-related factors, including
- Malnutrition
- Cardiovascular disorders
- Medication (e.g. non-steroidal anti-inflammatory drugs, corticosteroids)
- Obesity
- Microbial colonization of the wound
- Systemic disorders (e.g. diabetes, autoimmune conditions)
- Unrelieved pressure on the wound
- Maceration due to excess wound exudate or other moisture
- Inappropriate wound management
- Patient compliance with the wound care regimen
- Immobility.[6]
At the cellular level, many of these factors — such as diabetes, malnutrition, obesity and cardiovascular disorders — inhibit production and release of growth factors, macrophages and signal molecules to and within the wound bed. Alternately, if these cellular components are not present in the wound bed, this can give rise to other factors that stall healing, such as microbial colonization and excess wound exudate. Thus, a vicious circle can develop, keeping the wound in a state of low-grade inflammation, which requires appropriate wound management to restart healing.
We’ll explore these factors (and more) and how they impair wound-healing at the cellular level in another blog. However, this shortened list shows just how important it is to carry out holistic assessment of the wound and patient, so that challenges can be addressed. If they are not (and, sometimes, even when they are), wound healing can be impaired and delayed. The consequences of stalled wounds have far-reaching effects on patients and health systems alike.
Impact on patients’ lives
Stalled wounds can have a devastating impact on patient well-being that reaches far beyond the healthcare system and can compound healthcare costs. Although patients living with a wound are concerned with long-term healing, they may be more focused in the short term on reducing pain or odor, or being able to participate in their usual daily activities. Patients who cannot maintain or increase activity levels may experience a deterioration in the status of their wounds, and the social isolation that may come from living with a wound can result in anxiety and depression. As a result, patients may become non-concordant with treatment, leading to wound deterioration and the need for more advanced care over a longer duration. In addition, the management of mental health conditions further strains the healthcare system.
Impact for health systems
The cost of treating stalled wounds is significant. It’s estimated that, across Europe, 2-4% of healthcare expenditure — representing €6,000–€10,000 per wound, per year, and about £5 billion (€6.4 billion) in total annually —is spent on wounds, and this figure is on the rise.
Furthermore, stalled wounds are more likely to develop complications, such as infection, which in turn require more-costly interventions and more-frequent dressing changes, both of which place greater demands on our limited resources. In addition to higher costs, it’s estimated that between 25–50% of acute hospital beds are occupied by patients with a wound.
When patients are discharged into the community, hard-to-heal wounds pose further challenges in terms of distribution of resources. Longer healing times mean more dressing changes carried out by community and practice nurses. One study found 57 full-time nurses were needed for dressing changes alone in a community with a population of 288,000.[7,8] The per-unit cost of advanced dressings and products are not driving outsized wound care expenditures but, rather, the clinician time needed, particularly with challenging wounds where healing is prolonged.
Advanced therapies are needed
It’s inevitable that some wounds will stall during healing. When they do, it’s critical to recognise the markers — patient- and wound-related challenging factors, signs and symptoms of a prolonged low-grade inflammation phase — and change to an advanced therapy capable of restarting healing at the cellular level. Woulgan Bioactive Beta-Glucan Gel is an active wound healing product containing soluble beta-glucan (SBG), a proprietary substance shown to promote angiogenesis, cell proliferation and wound contraction by increasing production of key cellular components such as macrophages and cell-signaling molecules. Learn more here.
References
- Simon et al. Skin wound healing. Medscape, 20 January 2016. Accessed March 2016 at: http://emedicine.medscape.com/article/884594-overview
- Vowden P. Hard-to-heal wounds made easy. Wounds International, 2011. Accessed March 2016 at: http://www.woundsinternational.com/media/issues/514/files/content_10140.pdf
- Sheehan P, Jones P, Giurini JM, et al. Percent changes in wound area of diabetic foot ulcers over a 4 week period is a robust predictor of complete healing in 12 week prospective trial. Plast Reconstr Surg 2006;117(7 suppl):239S–244S
- Kimmel HM, Robin AL. An evidence-based algorithm for treating venous leg ulcers utilizing the cochrane database of systematic reviews. Wounds 2013;25(9):242–50
- Raffetto JD. The definition of the venous ulcer. J Vasc Surg 2010;52(5 Suppl):46S–49S
- The Royal Children’s Hospital Melbourne. Clinical guidelines (nursing): Wound Care. Accessed March 2016 at: http://www.rch.org.au/rchcpg/hospital_clinical_guideline_index/Wound_care/#factors_delaying_healing
- Dowsett C. Breaking the cycle of hard to heal wounds: balancing cost and care. Wounds Int 2015;6(2):17–21
- Lindholm C, Bergsten A, Berglund E. Chronic wounds and nursing care. J Wound Care 1999;8(1):5–10
love the article